Parenting
Is Cosleeping Really Unsafe?

This post was written in response to a question by TheScientificParent.org reader Kate.
It has been every parent’s worst nightmare for generations – finding their infant dead suddenly and unexpectedly. As a father of two, I remember the sleepless nights alternating between crying infants and complete silence, wondering if my boys were actually breathing. The fear is palpable. As a pediatrician who has had to pronounce infants dead and as a member of the team in my county that reviews infant deaths, I have far too often seen the grief and confusion when that fear becomes a reality.
For centuries we’ve struggled to understand the cause of, and even define what Sudden Infant Death Syndrome (SIDS) is. Over the years, the fear SIDS (sometimes known as cot death or crib death) has spawned multiple attempts by researchers and device makers to develop products to prevent SIDS – including apnea monitors, sleep positioners, or wedges. None of these interventions have been demonstrated to reduce the risk of SIDS. But what has been shown to reduce an infant’s risk of SIDS is very simple and many parents aren’t aware of it.
Since a consensus conference in 1991, Sudden Infant Death Syndrome (SIDS) has been defined as a death of an infant under one year of age that cannot be explained after a thorough investigation which includes an autopsy, a scene investigation, and a review of the medical and social histories. SIDS is one type of Sudden and Unexpected Infant Deaths (SUID). The reasons why the authorities need to investigate when an infant dies unexpectedly include ensuring no foul play was involved or whether or not a preventable genetic condition (like certain heart arrhythmias) occurred that impact future deaths in a family.
Improved death scene investigations over the past 2 decades have shown us that most SUIDs are a result of infants being placed in unsafe sleep positions. Improved examinations by death investigators and Child Fatality Review Teams have shown that for most infants who die of SIDS and a vast majority of infants who die of asphyxiation (also known as suffocation) or undetermined causes are found in an unsafe sleep position. The Back to Sleep campaign started in the 1990s after studies showed that infants placed on their back to sleep had a reduced risk of dying from SIDS. Between 1992 and 2001 the Back to Sleep campaign reduced the risk of SIDS by over 50%.
Unfortunately one of the worst sleep environments for a child is to co-sleep in an adult bed, or more specifically co-bed. We’ve designed adult beds to be comfy and welcoming for us at the end of a hard day, with pillows, blankets and soft mattresses, but these are all major asphyxiation risks for an infant not old enough to roll over or lift their head. Asphyxia while co-bedding can occur from 3 primary mechanisms – the parent rolling over on the child and restricting breathing, the child rolling or being rolled between the bed and a wall, or a child suffocating on soft bedding like blankets or pillows.
But these methods are not how most high-risk infants who asphyxiate while co-bedding die: Most die from carbon dioxide poisoning, by regularly re-breathing in their own or their parents exhaled breath. Any object near the mouth and nose of an infant can create an air pocket in which the exhaled air gets trapped. The infant then re-breathes air with a higher concentration of carbon dioxide. As the carbon dioxide level increases in the bloodstream and oxygen levels decrease, the infant is more likely to stop breathing and die.
These mechanisms for death can also occur in an adult bed without an adult and on other surfaces with an adult-like a couch. It is very easy for an infant to roll off the chest of a sleeping adult and get wedged between the parent and the side of the couch.
Due to an increase in the number of cases of Accidental Strangulation and Suffocation in Bed (ASSB), which have quadrupled from 1984-2004, the number of total infant deaths has stopped decreasing since 1998 despite the drop in SIDS cases. The number of deaths in unsafe environments, like co-bedding in adult beds, is staggering. A report out of Michigan in 2011 demonstrated that 83% of their infant deaths were a result of sleep related asphyxiation. Even looking only at SIDS cases, well designed epidemiological studies have demonstrated there is an increased risk of SIDS from co-bedding by itself after controlling for other risk factors, such as family history and smoking.
Despite the overwhelming body of research showing the deadly risks of co-bedding, many lactation consultants and some prominent anthropologists strongly believe co-bedding reduces the risk of death and increases the length of breastfeeding. While co-bedding may increase the length of breastfeeding and breastfeeding has been shown to independently reduce an infant’s risk of SIDS, the risks of sleeping in an adult bed outweigh the benefits gained by breastfeeding. Many co-bedding proponents claim that so long as the parent removes soft objects or strangulation risks from the bed (such as excessive throw pillows, heavy blankets or pillows and blankets with tassels) that co-bedding is safe. Unfortunately, these individuals have failed to understand the bigger picture and the lessons learned from Child Fatality Review.
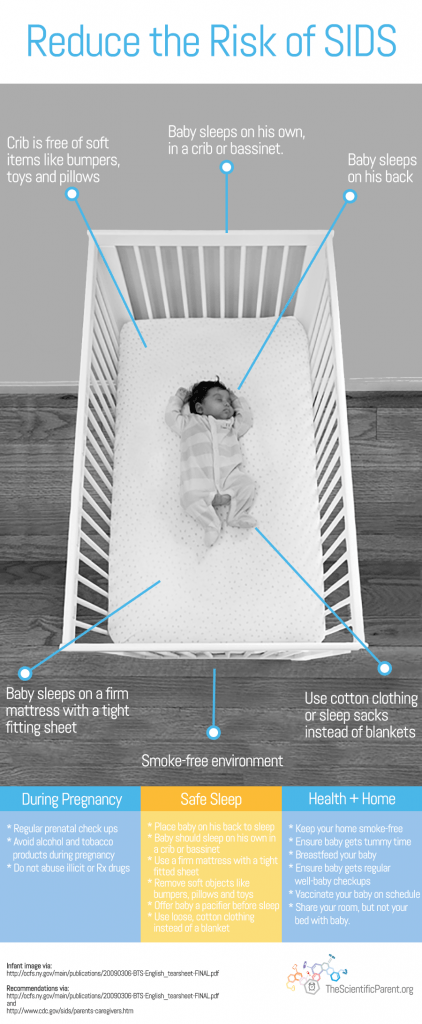
The American Academy of Pediatrics has several recommendations for parents who want to reduce their infant’s risk of SIDS and SUIDs, in addition to placing your infant on their back to sleep in a crib or bassinet of their own:
- Sleeping on a firm surface and avoiding soft objects in the crib
- Avoiding exposure to tobacco smoke
- Breastfeeding
- Room sharing without bed-sharing (place the bassinette next to the adult bed)
The research is clear: Very few infants die alone, on their back, and in a safe crib, and the majority of these deaths are preventable. I understand why some parents may want to co-bed or find themselves unintentionally co-bedding. Co-bedding can make parents feel closer to their infant, it also may make it easier for some parents to extend breastfeeding during the night and to get a little extra sleep. As a parent, I understand the exhaustion parents feel in the first weeks and months of life, and I’m not trivializing that, but the research is clear: Very few infants die alone, on their back, and in a safe crib, and the majority of these deaths are preventable.
For more information on safe sleep go to:
- Safe to Sleep: Public Education Campaign.
- Cribs for Kids: Helping Every Baby Sleep Safer.
- First Candle: Helping Babies Survive and Thrive.
- Reduce the Risk of SIDS.
- Center for Infant & Child Loss Safe Sleep Video
Resources:
- Safe to Sleep: Public Education Campaign. Led by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Accessed 06/22/2015.
- Cribs for Kids: Helping Every Baby Sleep Safer. Accessed 06/22/2015.
- First Candle: Helping Babies Survive and Thrive. Accessed 06/22/2015.
- Reduce the Risk of SIDS. Healthy Children,Org – by the American Academy of Pediatrics. Accessed 06/22/2015.
- Center for Infant & Child Loss Safe Sleep Video. Accessed 06/22/2015.
- Leslie Waghorn. Has A Seattle Doctor Found The Cause of SIDS? The Scientific Parent.
- Willinger, M. James, LS. Catz, C. Defining The Sudden Infant Death Syndrome (SIDS): Deliberations of an Expert Panel Convened by the National Institute of Child Health and Human Development. Pediatric Pathology. 1991 Sep-Oct;11(5):677-84. Accessed 06/22/2015.
- Ostfeld, B., et al. Concurrent Risks in Sudden Infant Death Syndrome. American Academy of Pediatrics. Vol. 125 No. 3 March 1, 2010
pp. 447 -453 (doi: 10.1542/peds.2009-0038). Accessed 06/22/2015. - The National Center for the Review and Prevention of Child Deaths. Accessed 06/22/2015.
- Laughlin, J., et al. Prevention and Management of Positional Skull Deformities in Infants. American Academy of Pediatrics. Vol. 128 No. 6 December 1, 2011 pp. 1236 -1241 (doi: 10.1542/peds.2011-2220). Accessed 06/22/2015.
- Kemp J.S., et al. Unintentional Suffocation by Rebreathing: A Death Scene and Physiologic Investigation of a Possible Cause of Sudden Infant Death. Journal of Pediatrics. 1993 Jun;122(6):874-80. Accessed 06/22/2015.
- Shapiro-Mendoza, C.K., et al. US Infant Mortality Trends Attributable to Accidental Suffocation and Strangulation in Bed From 1984 Through 2004: Are Rates Increasing? American Academy of Pediatrics. Vol. 123 No. 2 February 1, 2009, pp. 533 -539. (doi: 10.1542/peds.2007-3746) . Accessed 06/22/2015.
- Michigan Child Death State Advisory Team Tenth Annual Executive Report. 2011. Accessed 06/22/2015.
- Carpenter, R., et al. Bed Sharing When Parents Do Not Smoke: Is There A Risk Of SIDS? AN Individual Level Analysis of Five Major Case – Control Studies. Paediatrics. Volume 3, Issue 5. BMJ Open 2013;3:e002299 doi:10.1136/bmjopen-2012-002299. Accessed 06/22/2015.
- SIDS and Other Sleep-Related Infant Deaths: Expansion of Recommendations for a Safe Infant Sleeping Environment. American Academy of Pediatrics. Vol. 128 No. 5, pp. 1030 -1039. November 1, 2011 (doi: 10.1542/peds.2011-2284). Accessed 06/22/2015.
Author: Scott Krugman, MD, MS, FAAP
Originally posted at https://www.thescientificparent.org/crib-notes-is-cosleeping-really-unsafe/
